
Uploaded from the German Wikipedia, uploaded into the German Wikipedia by Der Lange on 7 November 2005, created by himself.
Science of Chess: A Case Study of Reflex Epilepsy Induced by Playing Chess
An electrical storm in the brain reveals links between chess and (some) other forms of complex thought.We're now three weeks into the semester at my home institution and my Neuropsychology students are just starting to try their hand at interpreting data from hypothetical (and a few real) brain-injured patients. That means that we encounter individuals with a range of circumstances that have affected the structure of their brain, including some truly sensational cases that involve things like fencing foils, tamping irons, and other improbable accidents. While the surreal injuries and rare diseases are often the things that capture my students' interest immediately, we ultimately spend a lot more time talking about much more common causes of functional disruption in the brain: Stroke, blunt-force trauma to the head, effects of chronic alcoholism, and the subject of this Science of Chess post - epilepsy.
I thought the case study I'll describe below was an intriguing subject for this series for a few reasons. Having written about fMRI studies describing a network of regions that support chess in the brain in the last two posts, I thought it would be nice to talk about some studies that use other cognitive neuroscience techniques. In particular, though I started my research career in an fMRI lab, I spent my post-doctoral work and the first few years of my faculty position using electrophysiological methods (specifically event-related potentials or ERP) to measure neural activity in infants, children, and adults. I'll say more about this technique in particular in a subsequent post, but suffice it to say that these two methods give us different, but complementary, information about neural processes: Broadly speaking, fMRI is great for answering questions about where things happen in the brain and EEG/ERP are good for answering questions about when they happen. As such, switching focus away from fMRI and towards electrophysiology seemed to me like an interesting next step for these articles. While reading up on some of this work, I came across this case report and thought it was an excellent example of how neuropsychological data (this time indexed using electrophysiology and behavior!) could reveal links between complex behaviors that help us understand something about how the mind is organized. That big idea - that the functional consequences of structural damage can help us understand how cognition is put together in the human nervous system - is what still makes me excited to teach this material to my students each year.
So, without further ado - let's take a look at our patient (and one or two other individuals facing similar circumstances), and see what they have to tell us about how the brain and the mind play chess.
What is epilepsy?
Our patient suffers from epliepsy, which I'm guessing is a term you likely have some familiarity with. In case you don't, however, you're in luck - Epilepsy is a condition that has been written about for milennia and one that we understand fairly well in terms of what is happening in the brain. Why it happens in the manner that it does for different individuals is still a very meaningful question to ask, but let's start by describing the phenomenon itself.
Briefly, epilepsy refers to a condition in which individuals experience recurring seizures. These can vary a lot both between individuals and within the same person at different times. Some seizures are characterized by large-scale shaking of the body and the loss of consciousness - thetonic-clonic or grand mal seizure, for example. Other seizures are best described as periods of cognitive absence, during which the individual may become unresponsive or "stare-y" but remains awake and exhibits no signs of tremor. Between these extremes, there a range of other outcomes that can include mood changes, muscle rigidity rather than tremor, transient confusion or "brain fog," or visual and auditory hallucinations or "auras." This wide variety of sometimes-dramatic symptoms is what led ancient science writers to describe epilepsy as "the sacred disease" or "falling sickness." Individuals with epilepsy can see things we don't see, become unable to speak while seemingly focused on something that isn't there, or experience whole-body convulsions with no discernible cause. A number of historically important figures that experienced vivid (and sometimes influential) visions accompanied by bouts of "possession" sound an awful lot like modern epilepsy patients if you read between the lines.
Hildegard of Bingen's visios of a "heavenly city" have many of the characteristics of the visual auras associated with some experiences of epileptic seizures. Image credit: https://worldneurologyonline.com/article/visions-or-auras-a-case-study-from-the-high-middle-ages/
An important point, however - many of those outcomes are things you may experience in the absence of a seizure, so don't start worrying that your occasional bout of mild cognitive stuck-ness means you're seizing. Likewise, seizures are not solely caused by epilepsy, so even if you or someone you know experiences clear seizure activity, this doesn't mean that they are epileptic. So what is the defining feature of epilepsy? Clinically, an epilepsy diagnosis generally depends on multiple instances of unprovoked seizures. That is, if you've definitely had seizures multiple times and there was no clear cause like an injury or a fever, you may be epileptic. But what do I mean by "definitely had seizures?" The physiological cause of the different outcomes I described above is abnormal, synchronous firing of neurons, or brain cells. That is to say, in epilepsy, sometimes large groups of brain cells start to produce activity altogether and that activity becomes large. Using electroencephalography (or EEG), we can measure that activity using electrodes placed on the scalp (see below). Voltage changes in the cortex lead to volume conduction of electricity through the brain, the skull, and the skin, until the fine wires inside each of the little pods you see on the sensor array below pick up a small change in voltage, generally on the scale of microvolts (or a millionth of a volt). The record we get of this activity during a seizure will probably look a lot like the image I chose for this article's title card.

By Chris Hope - https://www.flickr.com/photos/tim_uk/8135755109/, CC BY 2.0, https://commons.wikimedia.org/w/index.php?curid=24805878
The activity of those cells under typical conditions might lead you to move a limb, make an eye movement, or even see and hear particular things. During this unprovoked and synchronized bout of activity, however, the trouble is that those same behaviors can either be elicited by that neuronal firing when you don't want them to be (causing those muscle contractions and tremors I described above for example) and your ability to willfully do those things can be disrupted (leading to a transient inability to speak, for example). Further, because (1) neurons are little electrochemical devices and (2) electricity volume-conducts through neural tissue, strong, synchronized firing in a large group of neurons can lead to abnormal activity elsewhere in the cortex. This is what I was referring to up above in the sub-title when I talked about an "electrical storm" in the brain - though the generator of epileptic seizures may be focal (limited to one part of the brain), the effects of what happens there can spread, leading to a range of negative and debilitating outcomes.
What causes epilepsy?
That's what happens and how we measure it. But why does it happen? As I mentioned earlier, this is far trickier to answer. We know that there is a genetic contribution, so epliepsy is to some extent heritable. We also know that there are developmental syndromes that tend to increase the risk of epilepsy substantially. Epilepsy also can follow from brain injuries like stroke or blunt trauma. But these are all sort of distal causes - circumstances that set up the conditions that make an individual more prone to having epileptic seizures. What about more proximal causes? In the moment before an individual with epilepsy has a seizure, what happens that starts the cascade of events leading to the synchronous neural activity that will induce these sympoms? In some patients, a specific trigger - perhaps alcohol, stress, or exercise - reliably induces seizure activity. This sub-type of the disorder is called reflex epliepsy, to reflect the close relationship between some specific stimulus and the seizure activity. The extent to which a particular stimulus serves as a trigger may be related both to the generator of abnormal electrical activity in an individual's brain and the metabolic demands that the stimulus places on the nervous system. The patient we're going to talk about has a very particular trigger as it turns out - one that we can explore further to learn a little bit about chess in the brain.
The case study - Reflex epilepsy brought on by chess (and...?)
In reflex epilepsy, triggers can be simple or complex. A simple trigger might be photosensitivity, which refers to seizure induction from exposure to bright or high-contrast visual patterns. If you're a certain age, you might remember the hubbub about a Pokemon episodethat turned out to be a remarkably efficient (and accidental) trigger stimulus for some individuals. A more complex trigger, however, might be a particular kind of cognitive demand - doing a specific task might be the thing that leads to seizure activity. This is the case in the current patient we're considering, described in a case report by Mann et al. (2004). The individual in question suffered from mycoclonic jerks, or the quick convulsing of relatively small groups of muscles. If you've ever hiccuped, you've had a myoclonic jerk - similarly, if you've ever had that strange feeling of sort of twitching suddenly out of slumber (I always experience this as having landed on the bed after being dropped) that's also a good example.
The interesting thing about this patient's trigger for these movements, however, is that it was chess. There's a little more case history here, to be fair - as a teenager, this individual began experiencing myoclonic jerks in the upper arms, eventually followed by tonic-clonic seizures with some photosensitivity. These were controlled with medication, which was kept up until age 28, upon which the myoclonic arm-jerks reappeared - this time, with a very clear link to playing chess.
What is it about chess?
By itself, it's intriguing for chess to serve as a trigger, but it also makes me ask a lot of questions. What is it about chess that makes it the inducing stimulus? You could imagine a lot of possibilities: Perhaps chess exceeds some threshold of cognitive demand, putting metabolic stress on the nervous system? Does it have anything to do with the visual patterns used in chess matches? Chessboards are high-contrast and repetitive, after all - features shared by some visual stimuli that can induce seizures. Are there emotional components to the experience that are relevant to think about? Chess can be stressful cognitively and in terms of managing one's nerves - is chess a high-arousal or negatively-valenced event that makes those strong emotions serve as the trigger? The way to find answers to these questions (and maybe learn some neat stuff about cognition on the way), is to try and get as specific as we can about the manner in which chess serves as a trigger for this individual and the scope of activities outside of chess that may also trigger these symptoms. In both cases, there are some fascinating features of this patient's experience to consider.
First, it turns out that while the patient did experience myoclonic jerks of the arms while playing chess, the full clinical picture was a little more complicated than that. Those arm-jerks were largely confined to the middlegame and perhaps more importantly, were generally absent during the opening. That is, when this player is starting a game and presumably making moves on the basis of his memory for opening lines, nothing happens. Later, where there is more need to make decisions about possible moves, calculate what might happen in different lines, and evaluate the position - this is when we see those involuntary movements reappear. What does this mean? I wrote in a previous piece about memory-retrieval and problem-solving as complementary processes in chess skill, and this patient's experience of reflex epilepsy suggests that only of these two cognitive processes is linked to his seizures. Now we're getting somewhere - we're developing a picture of distinct cognitive processes that contribute to chess revealed by the differential relationship between opening play (memory), middlegame play (calculation? decision-making?) and seizure activity.
We can even go a little further and test this idea by asking the patient to try doing some other tasks while we measure what's going on in his brain and keep a careful eye out for arm spasms. The authors decided to try out the following collection of tasks, which make varying demands on memory, problem-solving, spatial calculation, and other processes: (1) Rey's Figure - a drawing task that involves both copying a complex figure and reproducing it from memory, (2) The Wechsler Memory scale - a standard neuropsychological memory test including subtests for different kinds of sensory memory, with and without delay periods, (3) Kohs cubes (see below) - a set of bisected red/white cubes used to solve spatial reconstruction problems based on matching a given 2D pattern, and (4) Raven's progressive matrices - a set of visual pattern recognition problems designed to test reasoning and problem-solving abilities. The pattern of behavior that we see from this patient across the opening phase of a chess game and later sections suggests that some aspect of chess problem-solving triggers seizures, not recalling chess moves. Which of these other tasks (if any) will also cause seizure activity? If none of them, then we may have to consider the possibility of some very specific locus for reasoning about chess and chess alone in the brain - if a few of them do induce seizures, however, looking at what these tasks share with chess might be an important clue to identifying a specific piece of the cognitive machinery that helps you play the game.
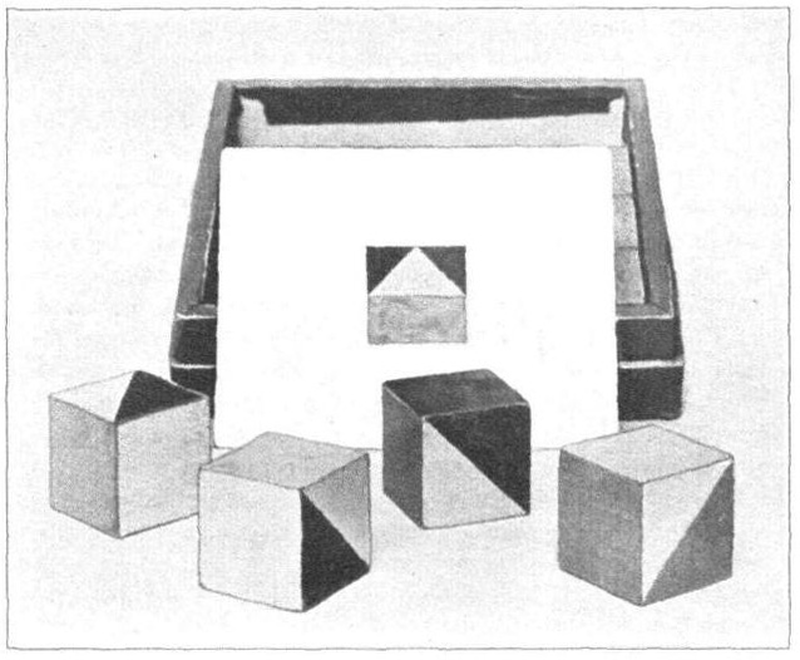
Kohs cubes - a reconstruction task for testing spatial manipulation, planning and pattern matching. By S.C. Kohs - Extracted from Kohs-Block-Design tests-1920.pdf, Public Domain, https://commons.wikimedia.org/w/index.php?curid=10217790
While recording both EEG activity from the patient's scalp and EMG activity from the patients's arms, a straightforward picture emerged as he carried out these tasks: Only manipulating Kohs cubes to try and solve them induced the convulsive movements of the arms. The same kind of activity was observed at the moment the patient would move his arm to make a move on the chessboard, clearly indicating that these tasks both served as a trigger for his epilepsy. Subjectively, the patient reported in each case that those involuntary arm movements sort of re-booted his thinking (he calls it "initialising" in the case report) and forced him to begin considering his actions all over again. This combination of objective measurement of task disruption and subjective report leads to a richer description of what might be happening: The process that evokes his seizures (and that is disrupted by them) has something to do with considering spatial actions to achieve a goal. If he's just remembering things - no seizures. If he's just trying to figure out the answer to a difficult visual problem (like the Raven's matrices) - no seizures. The key seems to be arriving at a series of movements that allows him to carry out some plan. Both the cubes and a typical chess middlegame require you to think about how to manipulate things in space to get what you want, including the actual body movements you need to make to achieve your goal. That may be the process that the two triggering tasks share, and what I think is sort of cool here is the link between the plan itself (e.g. I'll exchange knights, give check, then take the free pawn) and the actual motor plan that's connected to it (I'm going to pick up the knight on e4, move my hand over f6, drop it and pick up his knight...etc.). This connection between parts of cognition that we might have thought were more distinct is the kind of intuition-testing surprise that I love mostin the neuropsychological literature, because I think it's from these that we learn some of the most interesting things about the way we do the things we do.
Back-averaging to localize chess-triggered seizures
I want to close by linking what's happening to our patient (and why it might be happening) more closely to brain anatomy than I've done so far. EEG is generally not the greatest tool for localizing neural activity, but we do have a few tricks up our sleeve that make it possible to at least make some broad statements about both the where and the when of events in the brain. The authors employ one of these here called back-averaging, which is a means of using some event that you can pinpoint in time as the basis for examining the EEG signal preceding that event. In this case, the authors used the actual muscle movement recorded via EMG of the patient's upper arm as the time-locked event and then looked to see what the EEG signal was doing at that same moment (and a little before and after) across the different sensors in their array. To put it more simply, if the patient's arm just jerked - what was his brain doing at that same point in time? By collecting lots of snippets of EEG activity that are time-locked in this manner to the patient's myoclonic twitches, you can average those segments of brain activity together to try and work out what was measured at different parts of the scalp (on average) when these seizures happened. You can see the results of that averaging below.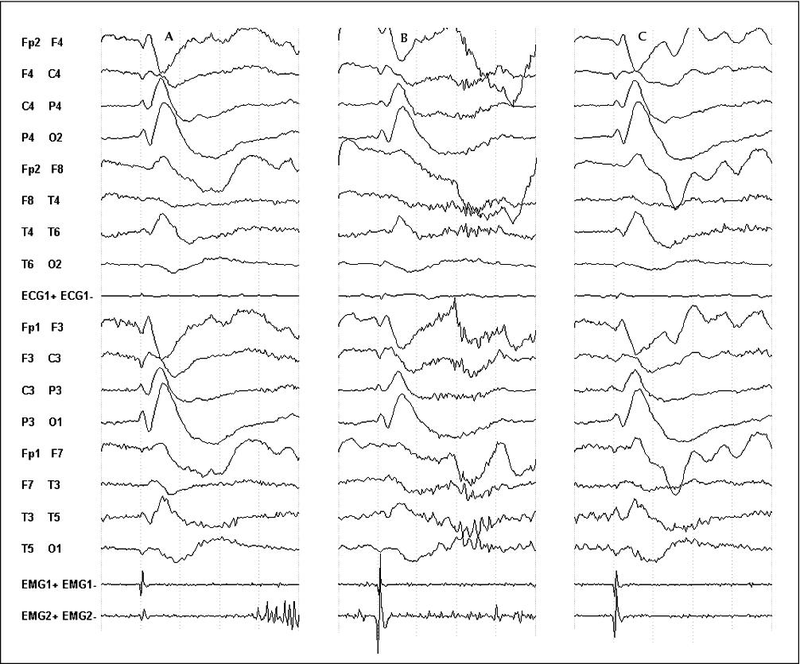
Back-averaging of the patient's EEG data (top 16 lines above) using spikes in the EMG (bottom two lines) to identify neural correlates of abnormal muscle activity. Large spikes over the electrodes mentioned in the text support a spatial-motor process that elicits seizure activity.
I've included a map of where these sensors are on the head to guide you, but the letters attached to them also help a little bit if you know some basic brain anatomy and terminology: F = frontal, C = central (right at the crown of the head), T = temporal (the sides of the scalp), P = parietal (approximately the top of the head, behind the crown a little), and O = occipital (the back of the head). The thing that I really hope stands out to you in this graph is that something BIG is happening in these averages over electrodes F3, F4, C3, C4, and P4 -which are largely over the frontal and parietal lobes. This is very coarse localization of where these spikes in brain activity are happening, but they are consistent with the regions in both of those lobes that we know support motor planning. To me, this is an interesting piece of supporting data that we're not talking just about a calculation or spatial reasoning process, but a process that also incorporates the act of moving to follow up on those calculations. Again, a potentially interesting and surprising insight into the connectedness of some cognitive processes during chess playing (calculating and moving your own body to enact a plan) and the separateness of others (memory and decision-making/problem-solving).
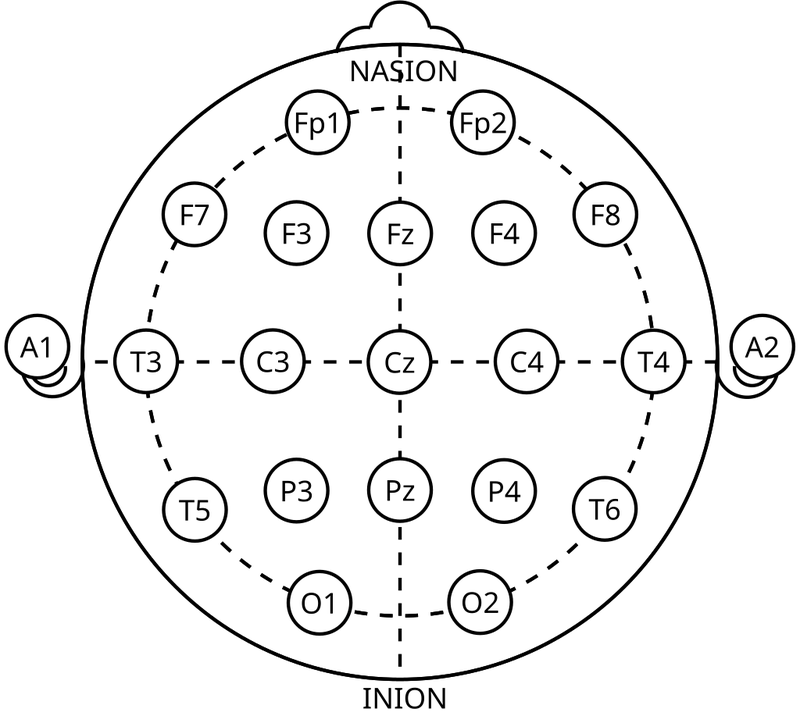
The 10-20 system of electrode placement. By トマトン124 (talk) - Own work, Public Domain, https://commons.wikimedia.org/w/index.php?curid=10489987
And there's more!
I'll add in conclusion that while this patient is indeed fascinating to read about, it's even more interesting to me that he's not alone! Down in the references you'll see links to some related case studies, some of which linking reflex epilepsy observed during chess to tasks like playing Shogi, playing Scrabble, or other kinds of complex cognition. The tricky thing about these kinds of case reports is that each one has the potential to tell us something very idiosyncratic about a particular player, but the picture across multiple patients also often helps us develop a clearer understanding of how some focal aspect of behavior is organized in the mind and the brain. I'm going to wrap this up for now because I'm literally off to lecture in about 30 minutes, but I hope you enjoyed this post and keep an eye out for more soon!
Support Science of Chess posts!
Thanks for reading! If you're enjoying these Science of Chess posts and would like to send a small donation my way ($1-$5), you can visit my Ko-fi page here: https://ko-fi.com/bjbalas - Never expected, but always appreciated!
References
Marín Gracia, M., Herrera Aramburu, M., Burneo, J. G., Debicki, D. B., & Suller Martí, A. (2024). Checkmate: Chess-induced reflex seizures in patient with juvenile myoclonic epilepsy. Epileptic disorders : international epilepsy journal with videotape, 26(1), 144–147. https://doi.org/10.1002/epd2.20156
Mann, M. W., Gueguen, B., Guillou, S., Debrand, E., & Soufflet, C. (2004). Chess-playing epilepsy: a case report with video-EEG and back averaging. Epileptic disorders : international epilepsy journal with videotape, 6(4), 293–296.
Marta Moreno, J., Mauri Llerda, J. A., Pascual Millán, L. F., & Morales Asín, F. (1992). Crisis epilépticas reflejas inducidas por el cálculo, juegos de cartas o de mesa y habilidades espacio-visuales [Reflex epileptic seizures induced by calculation, card or board games and spatio-visual abilities]. Neurologia (Barcelona, Spain), 7(1), 41–42.
Rey, M., Pelletier, J., Dalecky, A., Sabbagh, G., Levrier, O., Ali Chérif, A., & Khalil, R. (1996). Epilepsie réflexe avec crises induites par le calcul mental, le jeu d'échecs et le jeu de scrabble [Reflex epilepsy with seizures induced by mental calculation, playing chess and scrabble]. Revue neurologique, 152(2), 116–120.
Tatsuzawa, Y., Yoshino, A., & Nomura, S. (2010). A case of seizures induced by abstract reasoning. Epilepsy & behavior : E&B, 17(4), 552–554. https://doi.org/10.1016/j.yebeh.2010.01.020
You may also like
 CM HGabor
CM HGaborHow titled players lie to you
This post is a word of warning for the average club player. As the chess world is becoming increasin… NDpatzer
NDpatzerScience of Chess: Seeing the board "holistically."
Better players may read a chessboard in the same ways we recognize faces. Lichess
LichessShould I report this?
Ever encountered a user misbehaving on Lichess? Check out if and how to report them. NDpatzer
NDpatzerScience of Chess: Proving yourself wrong
The best players know it's not enough to be right, it's also working hard to find out when you're wr… CM HGabor
CM HGaborHow to make your chess training effective
This is the first post of a series about effective chess training. In the following posts, I will di… NDpatzer
NDpatzer